Services
3rd Party Liability
MAS routinely secures payment on Personal Injury Protection (PIP) benefits. Such payment is either secured directly from the insurance carrier or through the filing and enforcement of provider liens against patient recoveries for third party negligence.
Medical Accounts Systems’ staff will quickly and efficiently audit provider admission data to identify any account for which a third party may be financially responsible. Upon making this determination, MAS will identify the responsible parties, file and record the appropriate documents, and establish communication on a regular basis to ensure the provider’s charges are protected.
In addition to the foregoing, MAS, through its clinical denial program, will investigate, identify and properly substantiate partial denials by the carrier for services deemed unrelated to the compensable injury.
Finally, in the event that the third party is deemed to not be liable or the patient’s automobile insurance policy lacks med-pay coverage or has been fully exhausted, MAS will identify a secondary party to submit a claim for payment.
Case Study
Issue :
Auto carrier denied the claim indicating that the services provided to the patient were performed for a condition not related to the Motor Vehicle Collision (“MVC”) at issue.
Analysis:
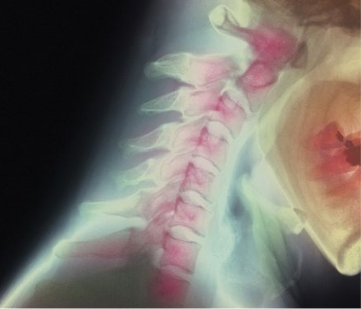
MAS reviewed the patient’s medical records and learned that the patient was involved in a MVC in 2016. The patient presented to an acute care facility complaining of right shoulder, right ribs, right lower back, and right ankle pain. The patient also indicated that he was experiencing generalized head pain, including a headache and neck pain. Due to the presenting symptoms and medical history of the patient, the attending physician ordered the patient undergo a CT of his head, as well as a CT of his cervical spine.
In 2018, the patient presented to same acute care facility, complaining of memory loss that he attributed to the 2016 MVC. Upon evaluation of Patient, the attending physician ordered the patient undergo an MRI of his brain, reasoning personality changes and memory loss as a cause for concern.
Utilizing the patient’s medical records, MAS crafted a detailed appeal identifying that the findings on the MRI clearly indicated that the patient’s symptoms were linked to the 2016 MVC. As such, MAS was able to establish that the MRI performed on the patient was, in fact, related to the prior MVC.
Solution:
The auto insurance company paid the deductible. The remaining balance was designated as patient responsibility. Subsequently, MAS facilitated the billing of the health insurance, which covered the balance as a secondary payer.